That. Smells. Awful
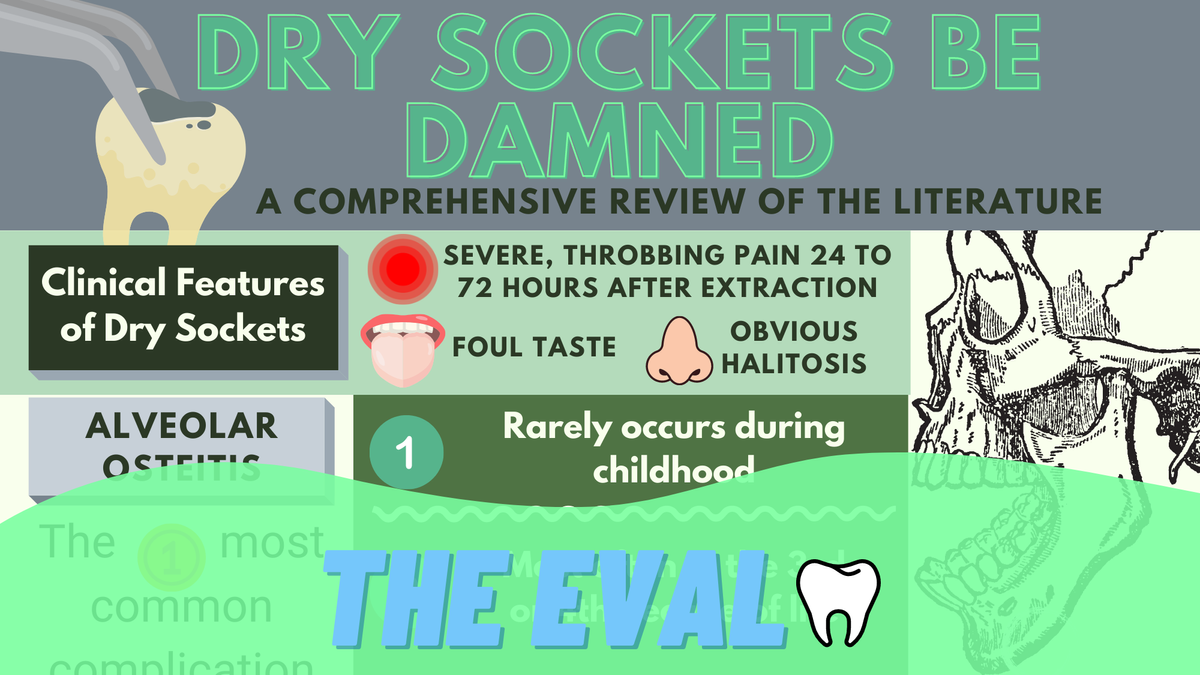
Call it what you will: dry sockets, alveolar osteitis, localized osteomyelitis. It's a pesky post-operative complication that most dentists will deal with at some point in their career. Here's your help- A Visualized Literature Review on all that you need to know to treat a smelly problem.
Nah, we aren't talking about anchovies.
In this case, we're talkin' dry sockets.
Dry sockets. Alveolar osteitis. Localized osteomyelitis. That pesky post-operative complication that makes your nose hairs burn as soon as it walks through your dental office doors.
“Don't use straws…”
...Shouldn’t be your only post-operative instructions after you take out those tricky mandibular molar teeth.
There is a whole bunch of information about the problem that causes your patients to look at you like, “what did you do to me.”
Everything you need to know…

An “Osteitis” search in the all-knowing PubMed will give you enough information to make your brain swell🧠. So here’s the latest updates that you need to know.
🔑The Keys. (All you visual learners skip this part and go straight to the infographic below👇)
- Watch the Mandible. Dry sockets occur 10 times more often in mandibular molars compared to maxillary molars
- Pesky Peri-coronitis. This one is important. It was found that 14.1% of patients with an already existing pericoronitis developed a dry socket (compared to 6.6% without the pericoronitis)
- Helpful and Simple. Current research shows that having your patients rinse with 0.12% Chlorhexidine for 30 seconds prior to the extraction decreases the incidence of osteitis by 50%.
- Summary. Unfortunately, the risk of alveolar osteitis is unavoidable, but factors that increase risk should be recognized. These include: gender, history of smoking, traumatic extractions, and age.
